The Truth About Neuroplasticity
Dr. Norman Doidge M.D. is a psychiatrist and a psychoanalyst. He has written many books including New York Times Best Seller, “The Brain that Changes Itself.” He also has written “The Brain’s Way of...

Neuroplasticity, from a clinician’s view, is the ability of the brain to change and heal itself. From a neuroscience perspective, neuroplasticity is the brain's ability to affect the synaptic transmission of information in response to external stimuli.
In this article, we will address…
At our concussion treatment center, we work with patients whose symptoms didn’t go away with rest and time. Neural plasticity is at the center of their recovery journeys. The brain’s ability to heal with therapy brings hope to our patients and to anyone else who has sustained a brain injury. Even those without injury or trauma can find an improved quality of life through neuroplasticity.
If you’re experiencing symptoms that won’t resolve after an mTBI, you’re not alone. And you’re not crazy. 90% of our patients show symptom improvement after just one week of treatment at our center specializing in neuroplasticity-driven therapy. To see if you are eligible for treatment, sign up for a consultation.

The Oxford Dictionary defines neuroplasticity as “the ability of the brain to form and reorganize synaptic connections, especially in response to learning or experience or following injury.” That said, the exact definition of neuroplasticity and all of the mechanisms behind it aren’t exactly settled science.
From a patient’s perspective, neuroplasticity is the brain’s ability to heal following injury when prompted by the right external stimuli. Most of the patients we see experience dysfunction in neurovascular coupling (NVC) pathways resulting from one or more concussions (or other forms of brain injury, such as transient ischemic attack, viral or bacterial infection, long COVID, carbon monoxide poisoning, and more).
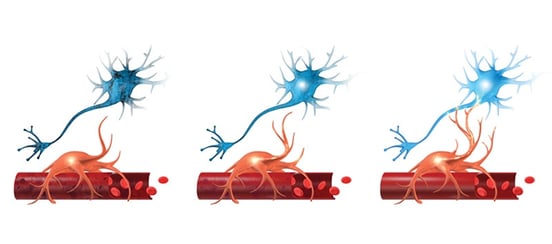
Neurovascular coupling (NVC) is the connection between neurons and the blood vessels that supply them with oxygen and other nutrients.
What does that mean, exactly? NVC refers to the connection between your neurons and the blood vessels that supply them with oxygen. Healthy neural connections will send chemical and electrical signals to “call” for oxygen whenever they need to complete a process; in response, more blood will flow to that gray matter. NVC is a delicate and dynamic process; even small changes in communication between neurons and these blood vessels can have negative consequences on brain function.
In the regions damaged by a concussion, the communication between brain cells and the blood vessels that supply them can be disturbed. Sometimes, a brain region might signal for too little oxygen to perform its task; in other cases, it might signal for (and receive) more oxygen than required, overtaxing your system and causing it to ‘burnout’ more quickly. The result is cognitive impairment.
With the right therapy, we can promote neuroplasticity in the affected neural network. This helps the brain to correct its signaling and use the right region for the right process and in the right way. Because of neural plasticity, your brain can restore connections to make that change happen.
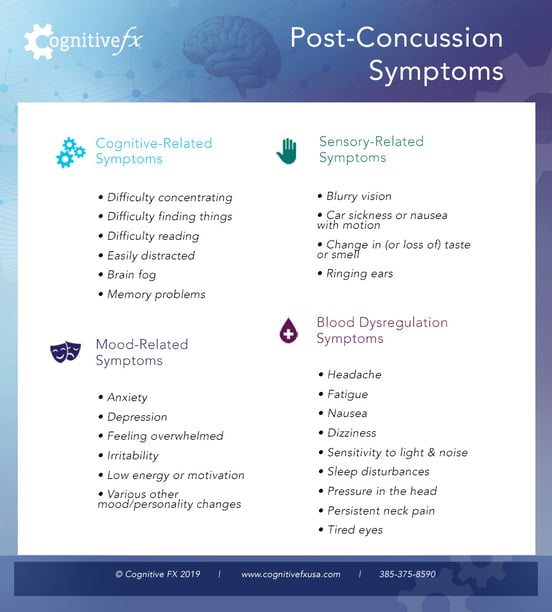
Some of the most common concussion symptoms that can result from poor neurovascular coupling include…
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
It’s normal for these symptoms to linger for a week or two after a concussion. But when they persist for more than three months, you likely have post-concussion syndrome (PCS). Fortunately, there are exercises you can do to encourage healing via neuroplasticity under the care and attention of a trained therapist.
Further reading: What can a neurology practice do for PCS and Types of head injury doctors

Neuroplasticity can work for or against you. If neuroplastic changes are in response to a persistent negative behavior or stimulus, that can make your condition worse. Likewise, neuroplastic reorganization can be harnessed to heal and lessen your symptoms — if you know what you’re doing. To understand how we use therapy to promote neuroplasticity, let’s examine the process we use at our clinic.

Every morning, the day begins with thirty minutes of aerobic exercise. Cardio jumpstarts your body and your brain, making it better able to respond to therapy that encourages healthy neuroplasticity. That’s because of the ‘post-exercise cognitive boost’ (PECB), in which a cascade of healthy neurochemicals floods the brain. One of the most notable neurochemicals released by exercise is brain-derived neurotrophic factor (BDNF), which has been shown to assist post-concussion recovery.

Not only does your body feel better, but with improved blood flow and neurochemicals from exercise, the brain functions better. That makes after a workout the perfect time to begin cognitive training.
Note: Many patients with PCS suffer from exercise intolerance. Fortunately, there are ways to exercise at the sub-symptom threshold (i.e., before it spikes severe symptoms). Learn more about safe post-concussion exercise.
At Cognitive FX, we use multidisciplinary therapy approaches, including…
 A therapist demonstrates using the Dynavision board, which challenges patients’ reaction times.
A therapist demonstrates using the Dynavision board, which challenges patients’ reaction times.
For example, Cognitive FX patient Sam Gray found this occupational therapy exercise to be memorable: balancing on the flat side of a Bosu ball while a trainer had him name a fruit for every other letter of the alphabet, beginning with the letter Z… All while they tossed a football back and forth.
 Balancing on a BOSU ball while engaging in cognitive exercises is just one example of therapy offered at Cognitive FX.
Balancing on a BOSU ball while engaging in cognitive exercises is just one example of therapy offered at Cognitive FX.
In his case, balancing on the BOSU ball was activating a subcortical region of the brain. The exercise targeted areas involved in visually assessing his environment, maintaining balance, and seeing himself in relation to the space around him.
Then, on the ball, he had to throw a football back and forth with his therapist, an ever-moving target. That activated areas involved in processes like visual tracking, visual search, hand-eye coordination, depth perception, and more.
Finally, the exercise included a memory recall aspect. In his case, it was naming fruits beginning with the letter Z, but it could be about anything from food to famous people. The idea is to perform activities that challenge the brain while also forcing multisensory systems to engage.
Obviously, the exercise described is more complex than something you might do on your first day of therapy. But it illustrates just how much you can do to engage brain plasticity.

Or, consider sensorimotor therapy. You might fight yourself clapping and stomping along to a metronome in a pattern given to you by your therapist all while playing Taboo or completing a visual search puzzle.
Note: The above examples are just a small fraction of the therapy exercises that we use to help concussion patients rewire their brains and heal from injuries. If you want to learn more about whether you could benefit from this treatment, schedule a consultation with our team.
Neuroplasticity rehabilitation is a stepwise process. You don’t jump into the hardest “brain training” exercises on day one. And you also don’t want to go from one cognitive exercise to another without rest.
In our practice, patients cycle through physical exercise, cognitive exercise, and rest multiple times throughout the day. You prepare the body with cardio, activate the brain as much as you can, and then rest until you’re able to do it all over again. Patients cycle through increasingly harder therapies throughout the course of treatment.
Breaks sometimes include using apps for binaural therapy (calming sounds and two distinct sound frequencies that your brain combines into a relaxing wavelength). Our patients also learn how to practice mindfulness and meditation.
It’s critical to have more than just one or two therapy sessions per week if you want the brain to use plasticity to heal itself, which is why we take the cycle of exercise and rest seriously.
Patients self-report symptom severity before and after treatment, and the results are remarkable. On average, patients improve 60% in their symptoms during the course of one week of treatment and continue improving once they’re home. But we don’t have to rely only on patient reports: We use fNCI to verify that neuroplasticity-based therapy is helping.
fNCI stands for “functional neurocognitive imaging.” It’s a type of functional magnetic resonance imaging (MRI) that shows blood flow in the brain. Brain activity is inferred by identifying blood flow patterns. Patients do cognitive tasks during the scan so we can see if each brain area involved in completing that task is calling for and using oxygen normally or abnormally.
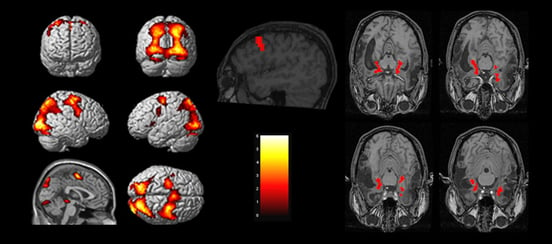 fNCI provides neuroimages to ‘see’ the results of neuroplasticity treatment at Cognitive FX in action.
fNCI provides neuroimages to ‘see’ the results of neuroplasticity treatment at Cognitive FX in action.
The scan images 56 brain regions and looks at communication between them. This type of fMRI provides a wealth of information that helps us understand what’s causing your symptoms.
For example, poor NVC in the hippocampus could lead to compromised neurogenesis and difficulties with different but recurrent short-term memory formation (such as remembering where you left your keys today instead of yesterday). Poor NVC in the basal ganglia, a subcortical structure found deep in the brain, could impact motor control, multitasking, emotions, and more.
The image below shows additional information about connections between brain regions. Certain brain regions talk to each other all the time; others rarely need to interact. Those that do talk have something like a highway of synapses that have strengthened their connections to each other. And when one region lights up, the others should light up in the same way. This part of the fNCI helps us to see which brain regions aren’t talking to each other as much as they should and which ones are talking to each other more than they should. That way, we can promote healthier connections during therapy.
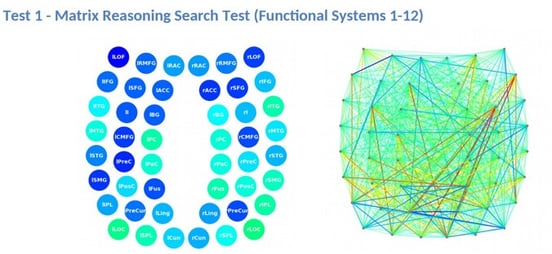
Some regions included in the scan are the left and right hippocampal areas, inferior frontal gyrus (IFG), and anterior cingulate cortex (ACC). Red shows over-connected regions; blue shows under-connected regions. In the scan above, for example, we can see that the right insula and the right inferior gyrus are overcommunicating. Maladaptive neuroplasticity after a brain injury can cause these communication changes in the brain.
The scan includes many cortical and subcortical structures, but cannot cover every part of the brain. For example, the fNCI can’t accurately assess pituitary gland or amygdala function.
In addition to fNCI, we also perform a structural MRI on the brain and cervical spine to ensure that your brain structures and bones are unharmed by your injury. If we do detect any structural changes, we will refer you to a neurosurgeon for further consultation.
Using fNCI means we have much greater specificity than most treatment providers because we know which brain regions to target during therapy. We also compare pre-treatment and post-treatment scans to verify functional changes in neurovascular coupling.

Neuroplasticity cannot be used to revive dead tissue in the brain, but it can be used to form pathways around it. There are a number of conditions and symptoms — such as cognitive decline from Alzheimer’s disease — that we do not treat in our clinic, but other clinics use neuroplasticity to improve the lives of those who suffer from these conditions.
But for most patients with mild traumatic brain injuries, understanding neuroplasticity can guide rehabilitation and facilitate improvement in symptoms stemming from the injury, ranging from attention difficultiesto balance issues to headaches. Cognitive function is significantly improved by therapy in most patients. However, there are some symptom categories we can’t specifically target or for which research is still nascent, such as migrainous headaches, primary mental health disorders, and hormone dysregulation.
Note: While we don’t treat patients with brain damage from severe traumatic brain injury during their acute recovery, we do work with them to help lessen the severity of long-term TBI symptoms. If you have lingering symptoms from a TBI and want to improve your quality of life, contact our team.
Our treatment plan is not designed to resolve mental health disorders that began before your injury. But any emotional symptoms that arose after your brain injury could improve if they are tied to neurovascular coupling, autonomic nervous system dysfunction, or the change in your quality of life due to injuring those areas of the brain.
The catch here is that there is very little research connecting neuroplasticity and improved emotional symptoms. Clinically, we have seen many patients’ emotional symptoms improve. But we don’t have a full understanding of why that is, and cannot make the claim that neuroplasticity is the direct cause for their improvement. To learn more about what we do know regarding these conditions, please visit these posts:
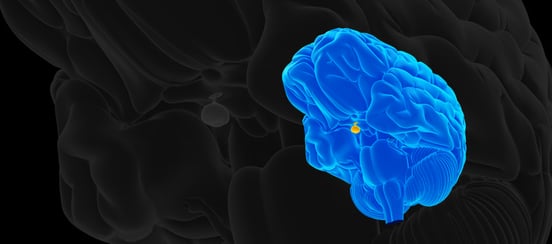 This image highlights the pituitary gland. Injuring the pituitary gland during a concussion can result in hormone dysregulation.
This image highlights the pituitary gland. Injuring the pituitary gland during a concussion can result in hormone dysregulation.
We often see patients who have many of the “traditional” post-concussion symptoms along with hormone problems. Maybe your cortisol levels get inexplicably low without necessarily being in adrenal failure territory. Maybe your child suddenly stopped growing and you’ve since learned that they aren’t producing enough growth hormone. Maybe you’re tired all the time and found out that low thyroid hormone is contributing to the problem.
If so, you’re in good company. There is a growing body of new research from clinical trials, research universities, and more to show that concussions can also cause hormone dysregulation (i.e., hormones that aren’t at the levels they should be when they need to be) due to changes in the function of either the pituitary gland or the hypothalamus.
In many cases, these hormones being “off” can cause many of the symptoms associated with post-concussion syndrome, from difficulty sleeping to exhaustion. But because research affirming that concussions can cause hormone dysregulation is so new, and because we can’t use fNCI to image the brain regions responsible for hormone production, we don’t have a way to treat these difficulties using neuroplasticity.
Further reading: Hormone dysfunction after a brain injury and How to talk to your doctor about hormone imbalance
For some patients, hormone deficits may improve after getting treatment for nearby parts of the brain. But many still need replacement hormones to finish the job. While we don’t prescribe those ourselves, we do refer patients to an endocrinologist for assistance whenever they need it.
As we continue our clinical practice, we hope to discover new and better ways to help these patients recover and thrive after treatment.
Note: One of our patients who experienced hormone dysregulation in conjunction with other post-concussion symptoms wrote about her treatment experience. We helped her feel better and have more energy; we’d love to help you, too. Sign up for a consultation to find out if you’re eligible for treatment at our clinic.

No matter where you go for treatment, there are a few ways to get the most out of your therapy sessions:
1. Embrace the will to make a change.
We’re not talking about optimism vs. pessimism here. But it helps tremendously if you consciously choose to do everything you can to get better. By cultivating the belief that you can and will change, you help your brain do what it needs to heal.
Positive thinking alone can’t heal the human brain. But when it’s combined with therapy that drives neuroplasticity in a positive direction, it’s a very powerful component in recovery.
2. Have a support system in place.
You don’t have to have amazing family and friends to recover, but having one or two people you can rely on during recovery makes a big difference. Could someone in your life travel with you to treatment? If not, are there ways they can help you prepare before you leave and readjust when you return?
Further reading: What family and friends can do to help TBI and mTBI patients and Support groups for post-concussion syndrome
3. Focus on addictions first.
Major addictions to drugs or alcohol can seriously inhibit treatment efficacy. We recommend that patients resolve existing addictions to the extent they are able before pursuing treatment. Otherwise, they are usually unable to give treatment their full attention — and their recovery suffers as a result.
Even hitting the caffeine too hard can make treatment difficult. We strongly recommend seeking therapeutic interventions for serious addictions before starting treatment, no matter where you choose to go for help.
Further reading: How alcohol and caffeine affect recovery from post-concussion symptoms
 Solving Sudoku puzzles probably won’t result in brain changes and new connections from neuroplasticity.
Solving Sudoku puzzles probably won’t result in brain changes and new connections from neuroplasticity.
While you can’t treat a brain injury alone, you can help your brain be at its best with certain practices. Contrary to popular belief, solving Sudoku puzzles isn’t really rewiring the adult brain or keeping it “plastic.” And it certainly won’t resolve symptoms from a head injury.
Fortunately, there are steps you can take at home to encourage a healthy brain prone to neuroplasticity.
Here’s a short list:
If you’ve sustained a mild traumatic brain injury — concussion or otherwise — and experience symptoms that won’t resolve on their own, neuroplasticity could be the key to your recovery. On average, our patients notice a 60% improvement in their symptoms after one week of treatment at our center specializing in neuroplasticity-driven therapy. Whether you’re an adolescent or older adult, neuroplasticity can still help.
To see if you are eligible for treatment, sign up for a consultation.

Dr. Alina K. Fong received her Ph. D. in Clinical Neuropsychology with an emphasis in neuroradiology from Brigham Young University. She received the national American Psychological Association Clinical Neuropsychology Division 40 Graduate Student Research Award in 2004 for her research on "Cortical Sources of the N400 and 'The N400 Effect." Dr. Fong's interest in brain mapping soon turned to functional MRI, and since then, her research efforts have been focused on the clinical applications of fMRI.

Dr. Norman Doidge M.D. is a psychiatrist and a psychoanalyst. He has written many books including New York Times Best Seller, “The Brain that Changes Itself.” He also has written “The Brain’s Way of...

Neurologists and Neuropsychologists often get mistaken as one and the same. Although there are some similarities, the differences...